Knowing that Covid-19 patients could be discharged after a certain number of days with no danger of infecting others could free up healthcare resources for other purposes, experts said.
A local multicentre study of 73 patients of various ages may make it possible to modify the country's discharge policies. It found that although patients still had the virus in their bodies 11 days after they first fell ill, the virus was no longer viable, as it could not be isolated or cultured in a laboratory.
The study's results were revealed in a position paper by the National Centre for Infectious Diseases (NCID) and the Academy of Medicine's Chapter of Infectious Disease Physicians.
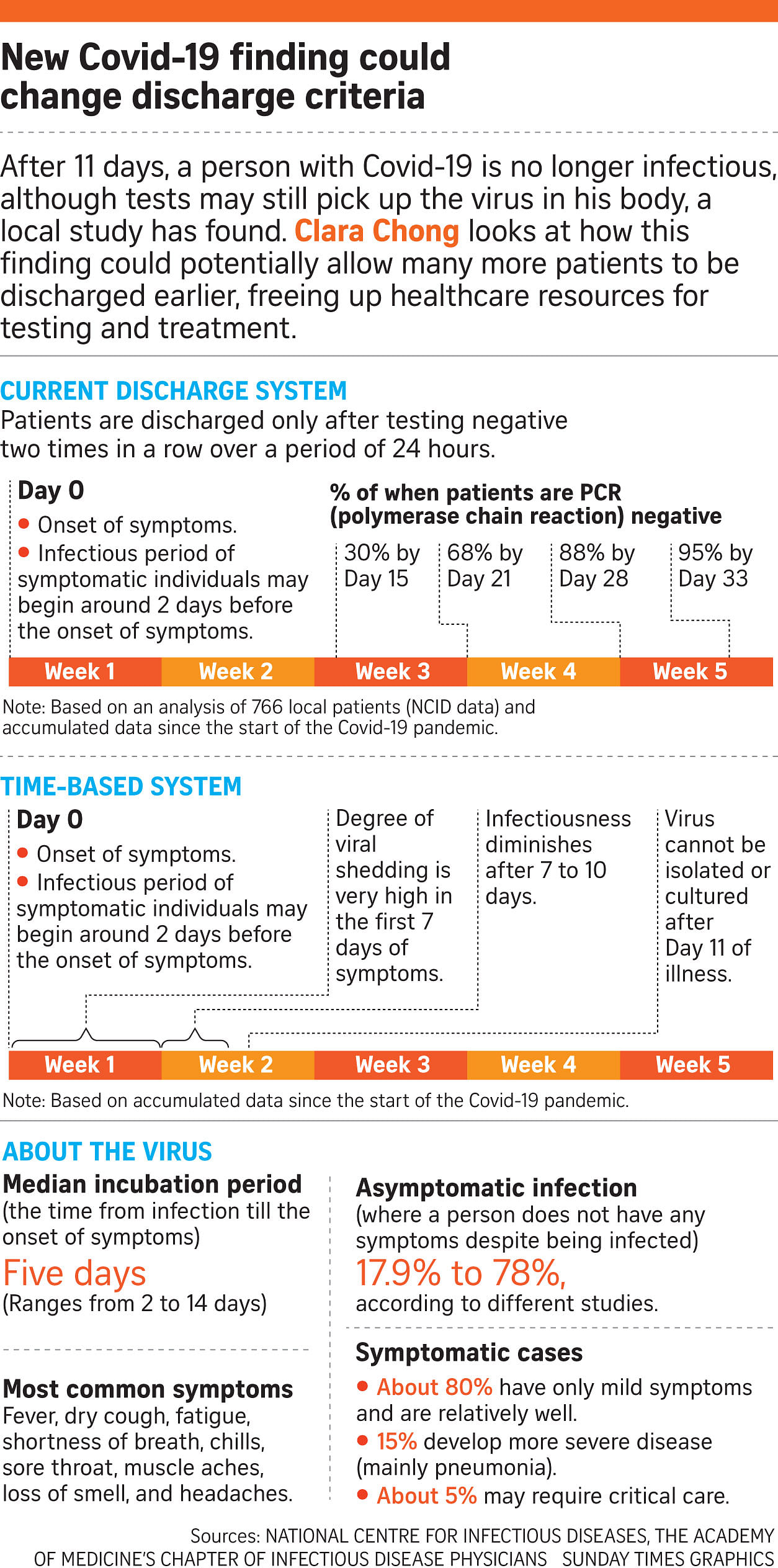
In Singapore, patients have needed two negative swab tests, 24 hours apart, in order to be discharged - even if they have not been sick for some time.
But on May 15, 18 patients were discharged from the D'Resort community isolation facility without those consecutive tests after they were deemed to be non-infectious to others. They had been in the facility between 38 and 51 days.
The need for two consecutive negative tests has resulted in large numbers of patients held in the community care facilities (CCFs) and hospitals beyond three weeks, all of whom have recovered fully from the infection, Associate Professor Hsu Li Yang, programme leader for infectious diseases at the National University of Singapore's Saw Swee Hock School of Public Health noted.
"If we use a time-based discharge policy of two weeks from onset of infection or first positive test, then the CCFs would be emptied out faster. More healthcare workers and administrators can also be freed up for other duties."
These could include doing more testing in the community for undetected infections, or testing more people with acute respiratory symptoms.
Professor Leo Yee Sin, executive director of the NCID, said the swab samples from the 73 patients were tested in a high-security Biosafety Level 3 laboratory. No matter whether a patient had a mild or a severe form of the disease, none remained infectious by the 11th day of their illness.
The discharge policy can now be revised according to this position paper, said infectious disease physician Asok Kurup from Mount Elizabeth Hospital.
"We may be able to divert the resources and get more testing done in the earlier stages rather than in the last," Dr Kurup said.
An aggressive testing strategy will also speed up the detection of cases and contact tracing, even during the pre-symptomatic phase, helping to nip transmission, he added.
However, the loosening of the Republic's discharge policy does not come without risk and would depend on how conservative the authorities are, said Professor Dale Fisher, a senior infectious diseases expert at the National University Hospital.
"You look at the science, bearing in mind that science isn't 100 per cent right, factor in how much insurance you want to build in and choose a day of discharge that is safe and efficient," he said.
But there is also room for flexibility, Prof Fisher added. "It is possible that there could be something in between, a certain number of days in supervised isolation, isolation facilities and hospitals, and maybe home quarantine subsequently as insurance.
"As we learn more about the virus, we are evolving and able to apply what we know. It was a good strategy before, but we can now figure out a better way to do it," he said.