SINGAPORE – Cholesterol has a bad reputation, but the waxy, fatty substance is needed to build cells, produce hormones and boost brain health.
In fact, the brain is the most cholesterol-rich organ in the body, containing 20 per cent of the substance.
But little is understood about how cells such as neurons contain the right amount of cholesterol needed. Abnormal distributions of cholesterol in the nerve cells have been linked to Alzheimer’s disease and other forms of dementia.
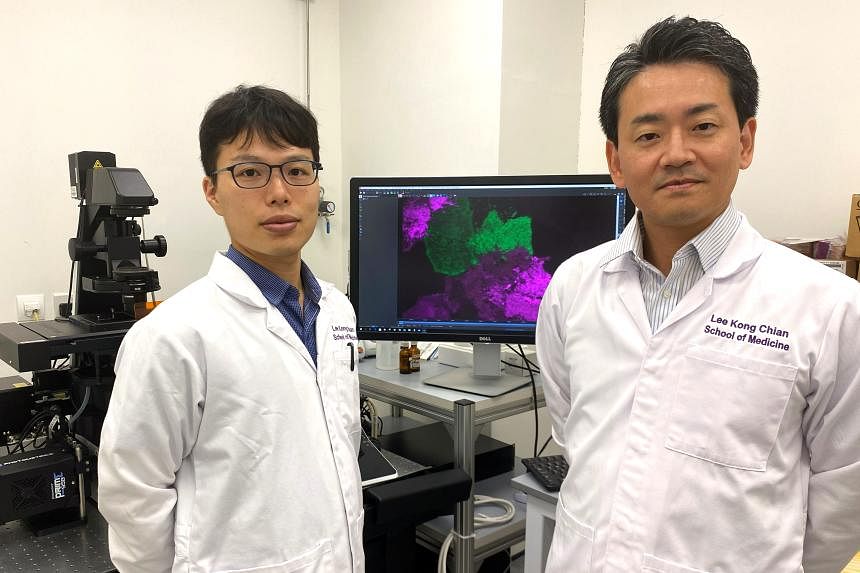
Over three years of peering at cells through a microscope, four scientists from Nanyang Technological University’s (NTU) Lee Kong Chian School of Medicine have uncovered three key proteins and their mechanisms that control the amount of cholesterol and how it moves within a cell.
They suspect that these proteins may not be communicating the way they should for people who have heart disease or dementia. Some of the proteins could be missing or in excess, for instance.
“The study has implications in terms of understanding the development of neuro-degenerative disorders and cardiovascular disease, which are highly associated with the abnormal distribution of cholesterol,” said the study’s lead, Associate Professor Yasunori Saheki.
He is hoping that the proteins can be further researched and used in future therapies against such diseases. For example, if it is possible for scientists to detect a protein going haywire before it affects cholesterol in a neuron, they could work on targeted solutions to restore the protein’s functions.
Prof Saheki, who specialises in cell biology and neuroscience, noted that there is currently no cure for Alzheimer’s nor good biomarkers available to predict the disease.
High-cholesterol diets increase cholesterol levels in blood, which can eventually lead to heart attacks and stroke. Among people with high cholesterol, a small portion of them cannot react well to cholesterol-reducing drugs because they lack the receptors that enable the cells to take in the substance.
The researchers used a protein-based cholesterol probe, or sensor, to visualise cholesterol distribution in the cells. Doing this, they identified three proteins, called ORP9, OSBP and GRAMD1, and observed that these control the distribution of cholesterol in cells.
Research fellow Tomoki Naito, the study’s first author, turned the proteins on and off in the cell to uncover each protein’s pathway and behaviour.
When ORP9 is deactivated, OSBP becomes hyperactive, leading to excessive amounts of cholesterol transported to other parts of the cell, disrupting its distribution. And cells without the GRAMD1 protein had an abnormal distribution of cholesterol in crucial parts of the cell, such as the cell membrane.
Commenting on the study, Professor Tan Huay Cheem, a senior consultant at the National University Heart Centre, Singapore, said: “Should some of these proteins be deactivated or deficient, some form of gene-modifying therapy re-introducing these proteins could help. GRAMD1, if deficient, could perhaps be re-introduced in the form of injectables that can hopefully be taken up by the cells.”
But he stressed that these clinical possibilities are still speculative.
The team’s findings were published in the scientific journal Nature Communications in September. The study was done in collaboration with two researchers from the NTU School of Biological Sciences.
The team plans to study diseased cells from Alzheimer’s or heart disease patients to further investigate how the proteins behave in those cells. They may obtain the cells from a consortium in the United States or from colleagues here who work on human genetics.
“We know there are missing components in our understanding, and we want to discover that. We think we have built foundational knowledge that is sufficient to answer the question of how neurons distribute cholesterol, which is an age-old mystery,” said Prof Saheki.
Associate Professor Guillaume Thibault, a cell biologist from the School of Biological Sciences who is not involved in the study, said: “The next logical step is to investigate whether modulating these key proteins can restore normal cholesterol levels in disease-affected cells. Such research could pave the way for innovative therapeutic strategies targeting a range of cholesterol-related diseases.”
He added that while there is some way to go before the research reaches the clinical stage, it is an important step forward.
Prof Tan said: “Modern medicine advancement is often rooted in foundational basic science research. For clinicians like myself, we are always looking for a therapeutic agent that can potentially lower the amount of bad cholesterol in the blood.”